Geographical analysis
Department of Geography & GIS
Department of Geography & GIS
Geographical analysis
DOI: 10.53989/bu.ga.v14i1.24.197
Year: 2025, Volume: 14, Issue: 1, Pages: 54-66
Original Article
Amritpal Singh1, L T S Guite1∗
1Department of Geography, Central University of Punjab, Punjab, India
*Corresponding Author
Email: [email protected]
Received Date:17 October 2024, Accepted Date:10 August 2025
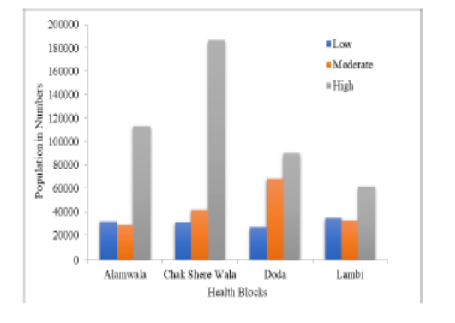
Mosquito-borne diseases are those that are transmitted by the bite of an infected mosquito. Stagnant bodies of water are frequently preferred as mosquito breeding places. However, from producing eggs to the final stage, several elements contribute to its incubation, maturity, and growth to the point where it is capable of biting and transmitting diseases. The primary goal of this research is to focus on connected environmental determinants that provide optimal breeding locations and vulnerability mapping of mosquito-borne diseases using geospatial techniques and a decision-making approach. The analytical hierarchy process was combined with a geographic information system to create a map of mosquito-borne diseases in Muktsar district of Punjab state. The weights of selected variables were determined using a choice-based varied ranking method, which involved building a pair-wise comparison matrix. Initially, ten important environmental parameters were selected to determine their weight using a pair-wise comparison matrix. At the same time, the weight of each related element was employed as a geo-database to aid with overlay analysis. The consistency ratio was derived to evaluate the decision-making process and significance measurement. The consistency ratio of choice factors was found to be 0.0470, which is less than 0.1 and regarded consistent and acceptable. According to the study's findings, proximity to water bodies is a major influence, followed by moisture content, water index, availability of shade area, and the presence of vegetation in mosquito-borne disease prevalence. The current findings demonstrate the wide range of uses of satellites data and spatial techniques in epidemic diseases zonation.
Keywords: Mosquito-borne diseases, Geospatial analysis, Analytic Hierarchy Process, Public health
© 2025 Singh & Guite. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Published By Bangalore University, Bengaluru, Karnataka
Subscribe now for latest articles and news.