Geographical analysis
Department of Geography & GIS
Department of Geography & GIS
Geographical analysis
DOI: 10.53989/bu.ga.v14i1.24.256
Year: 2025, Volume: 14, Issue: 1, Pages: 77-87
Original Article
Tanmoy Basu1∗, Biraj Kanti Mondal2
1Faculty (State-Aided College Teacher, Category-I), Department of Geography, Katwa College, Katwa, Purba Bardhaman, 713130, West Bengal, India
2Assistant Professor, Department of Geography, School of Sciences, Netaji Subhas Open University, Kolkata, 700064, West Bengal, India
*Corresponding Author
Email: [email protected]
Received Date:06 December 2024, Accepted Date:10 August 2025
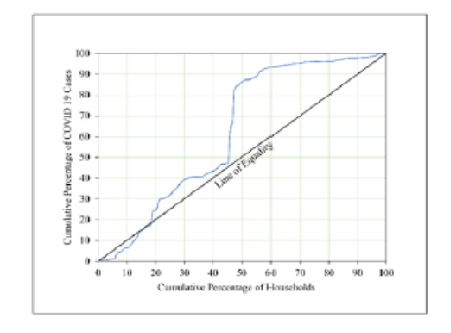
This present study assessed the health inequalities and evaluated the relationship between urban development and pandemic vulnerability through the Composite Ibrahim Index (CIb) and framed the blueprint of multiple socio-economic drivers in the Kolkata Municipal Corporation (KMC) of India. The COVID-19 pandemic exacerbated pre-existing health and socio-economic inequalities across urban India, and Kolkata, being a leading megacity of India, conceptualizes its health as an emerging and critical hotspot area of investigation. The primary objective is to analyze spatial patterns of COVID-19 vulnerability across 141 wards of KMC and identify key determinants influencing household-level health inequality. Secondary data were sourced from the Census of India, the Bureau of Applied Economics and Statistics, and KMC records, and analytical techniques included time-series analysis (3-month moving average), Lorenz Curve, and Gini coefficient (0.75 indicating high inequality), Composite Z-scores, and multiple linear regression with marginal effect analysis. Results indicate that highly populated and socio-economically weaker wards, such as 31, 33, 66, and 70, reported higher active cases, while development status and COVID vulnerability showed a significant negative relationship (R² = 0.05, p < 0.001, N=141). Drivers such as open latrines, dilapidated housing, and households with no sanitation or drainage significantly reduced CIb values, while overcrowding increased vulnerability. The study concludes that socio-economically underdeveloped wards are disproportionately affected, and the null hypothesis of no relationship is rejected. As a policy measure, sustained vaccination, hygiene awareness, targeted urban health interventions, and strengthening of the National Urban Health Mission are essential to mitigate inequality and ensure resilient urban health systems. A data-driven, integrative approach is necessary for future pandemic preparedness in the context of rapid urbanization and sustainable management of Kolkata.
Keywords: Health inequality, Pandemic, COVID-19, Ibrahim index, Regression, Drivers, Kolkata
© 2025 Basu & Mondal. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Published By Bangalore University, Bengaluru, Karnataka
Subscribe now for latest articles and news.